Table of Contents
Do you know that 14% of office-based physicians still rely on paper records? Even though the healthcare landscape is going through a paradigm shift, many of them are not implementing it. This is mostly because of the illiteracy of such innovations.
Electronic health records (EHR), one such system, have become indispensable tools for healthcare organizations to manage patient data efficiently. However, the path to successful EHR implementation begins long before the technology installation.
Comprehensive training and onboarding of staff lay the critical groundwork for your organization to fully leverage these electronic health record systems.
How Does an EHR System Work to Enhance Patient Care?
Before diving into EHR training best practices, it is important to understand what EHR systems are and how they work.
EHR systems are digital versions of patient health information, including medical history, diagnoses, medications, treatment plans, immunization dates, allergies, radiology images, and laboratory test results. This electronic health records system replaces traditional paper medical records to provide real-time, patient-centered records that can be easily accessed by all healthcare providers involved in the patient’s care.
The core purpose of EHR systems is to streamline and improve the management of patient health data to enhance clinical decision-making and the quality of care. Benefits include:
- Improved access to patient records for authorized healthcare providers.
- More coordinated care between interdisciplinary care teams.
- Reduced medical errors due to poor legibility or availability of paper charts.
- Increased patient engagement through patient portals.
- Enhanced care quality and outcomes through proactive treatment and analytics.
Understanding the EHR systems meaning and their significance, is paramount for effective utilization post-implementation, ensuring staff can maximize these advantages seamlessly. This elucidates the essence of EHR systems, delineating their pivotal role in modern healthcare delivery. With the right strategies, your staff can leverage these advantages fully after EHR implementation.
Evaluating and Supporting EHR Trainers
The effectiveness of your training program relies heavily on the skills of the trainers guiding staff. Considerations for assessing and optimizing EHR trainers include:
- Subject Matter Expertise: Evaluate their functional & technical knowledge through testing and credentials. Trainer gaps need to be addressed.
- Instructional Design Skills: Assess their ability to translate complex topics into focused, easy-to-understand sessions.
- Delivery Skills: Observe training sessions to ensure they keep learners engaged through effective presentation skills, pacing, and audience interaction.
- Continuous Development: Provide ongoing learning opportunities to trainers on instructional design approaches, adult learning principles, coaching skills, and platform knowledge.
- Feedback Channels: Gather regular input from learners on trainer quality and incorporate comments into improvement plans.
- Success Metrics: Track trainer performance based on metrics like learner proficiency improvements, training satisfaction, and knowledge retention over time.
- Toolkit: Equip trainers with resources like slide decks, job aids, simulation scenarios, and exercises tailored to each staff role.
- Recognition: Celebrate and reward trainers who consistently deliver excellent training experiences and outcomes.
Investing in your training team ultimately translates into a more confident and proficient end-user community equipped to leverage EHR systems optimally. Now let’s explore best practices for training and onboarding teams effectively.
Best Practices for Training and Onboarding Teams
Conduct Readiness Assessments for Implementation Success
The first step is to objectively evaluate your staff’s readiness to adopt the new EHR system. This includes assessing:
- Technological skills: Conduct skills testing to identify gaps in computer literacy, typing speeds, and digital capabilities.
- Learning styles: Evaluate how staff prefer to learn – visual, auditory, reading/writing, kinesthetic, or mixed – to develop appropriate training approaches.
- EHR experience: Determine the proficiency levels staff already have with existing or legacy EHR systems.
- Perceptions: Survey expectations, concerns, and motivations staff have about the new system. This proactively flags potential barriers like change resistance.
Tools like questionnaires, focus groups, and competency assessments can uncover readiness levels and shape a customized implementation strategy.
Create Tailored EHR Training Programs for Each Learner
With diverse roles and learning needs on your team, customized EHR training is crucial for assimilating new skills. Build targeted lesson modules to teach:
- Basic computer operation to new users, if needed
- Core EHR functionalities like data input and patient record navigation
- Specialized workflows as per provider roles – physician, nurse, admin, etc.
- Compliance training on data protection and privacy protocols
Training methods can include:
- Instructor-led sessions for foundational knowledge
- Interactive tutorials for self-paced learning
- Simulations to practice workflows.
- Visual aids like videos and process maps
- Leverage EHR Vendor Experts to Enrich Learning
EHR vendors understand their software intricately. Collaborate with them to provide:
- Super-user training for your IT staff who will support users
- Webinars and workshops on advanced system features and updates
- Help resources like user manuals, eLearning modules, and contact support
- These supplement your organization’s internal training team to upskill staff extensively.
Training Staff on EHR System Updates
As EHR products evolve via patches, upgrades, and new versions, it is critical to train staff on navigating these changes:
- Assess features being added/updated and identify associated workflows.
- Develop release notes and user guides for changes.
- Deliver targeted training on new capabilities.
- Provide refresher courses on changed aspects of existing features.
- Gather user feedback to refine training approaches continuously.
Keeping staff skills current on system updates through ongoing education ensures they can leverage EHR enhancements to continue improving patient care.
Adopt a Phased Approach with Ongoing Support Structures
Rather than overwhelming learners with everything at once, conduct training across multiple phases:
- Phase 1 – Fundamentals: Basic Computer Orientation and Introduction to EHR.
- Phase 2 – Core Workflows: Key Work Processes for Each Staff Role.
- Phase 3 – Optimization: Advanced Tools to Maximize Productivity.
- Phase 4 – Upgrades: New feature training with version updates.
Ongoing support structures like help desks, how-to guides, and refresher training help sustain proficiency post-implementation.
Incorporate Real-Life Practice Scenarios and Patient Data
Classroom training alone is insufficient to ingrain new EHR skills. Provide supervised opportunities for staff to simulate workflows using:
- Test patient cases mirroring actual documentation needs
- De-identified patient data from your organization to simulate real-world complexities
- Equipment like laptops or tablets where the system will be used
This applied practice builds confidence and readiness for go-live transitions.
Design Comprehensive Assessments to Gauge Training Effectiveness
Kirkpatrick’s training evaluation model provides a structured approach to measuring effectiveness across four levels:
- Reaction: Evaluate learner satisfaction with training delivery and content.
- Learning: Test knowledge and skills acquisition through quizzes or proficiency tests.
- Behavior: Assess skill application and process adherence on the job through audits.
- Results: Evaluate success metrics like productivity, patient outcomes, and downstream ROI.
Ongoing assessments identify training gaps to address through refresher courses.
Motivate Continuous Learning and Evolution
The EHR landscape evolves constantly, underscoring the need for continuous staff education. Some strategies include:
- Gamification with points or leaderboards to motivate engagement
- Microlearning through short, focused video tutorials
- Peer training to exchange best practices
- Mandatory annual training on upgrades and feature enhancements
- Rewards for completing voluntary, advanced courses
This habituates staff to be adaptable lifelong learners even after the initial rollout.
Ensure Leadership Support and Buy-In
- Highlight EHR training as a strategic priority with leadership endorsements.
- Define executive sponsors and project champions to promote engagement.
- Allocate a sufficient training budget and resources.
- Lead by example, with managers undergoing training first.
EHR adoption cannot happen in silos. Visible leadership commitment maintains priority amid competing demands and motivates staff participation.
Promote Networking and Knowledge Sharing
- Create online forums/groups for staff to discuss training experiences.
- Host “lessons learned” sessions for teams to exchange implementation insights.
- Enable shadowing opportunities across departments learning the system.
- Recognize and reward staff who proactively share EHR knowledge.
Collaborative learning beyond formal training amplifies growth and taps insights from peers navigating similar challenges.
Develop End User Engagement Strategies
- Communicate benefits of EHR adoption and how it improves work.
- Involve staff in aspects like goal setting and input on workflows.
- Create EHR utilization targets and friendly competitions.
- Share success stories and wins resulting from the use of the system.
Engaged end users who understand the value of EHRs are more motivated to learn and utilize them effectively.
Evaluating EHR Training Effectiveness
To ensure your electronic health records (EHR) system training translates into genuine learning and proficiency gains, focus on assessing learners across these dimensions:
- Pre-training assessments: gauge baseline knowledge of the EHR system through tests to quantify improvement.
- Learning verification: Use quizzes, assignments, or skills tests to confirm understanding of core EHR workflows.
- Workflow adherence: audit learners on following EHR protocols taught during training.
- Accuracy: Evaluate performance quality by reviewing learner work products completed using the EHR, like patient charts.
- Speed: Assess if learners complete EHR tasks more quickly by tracking time-on-task before and after training.
- Satisfaction surveys: Get feedback on EHR training experience and areas for improvement.
- Patient outcomes: Link key metrics like readmissions to EHR proficiency levels.
- Cost/benefit analysis: Compare EHR training costs to productivity gains and ROI.
- Refresher training: Use assessment data to provide targeted supplemental training on problem EHR areas.
Ongoing learner evaluations through varied tools provide tangible evidence of how well the EHR training translated staff skills and achieved the core purpose of improving clinical workflows and patient care.
The Costs of EHR Training
The costs associated with comprehensive EHR training should be factored into the overall implementation budget. Key considerations include:
- Vendor-led training and custom content development fees
- Ongoing training department overhead
- Staff time away from clinical duties during training
- Supplementary learning resources and tools
- Continuous education on new EHR features and upgrades
According to one study, a multi-physician practice may spend around $85,000 on first-year EHR training and support alone. While not insignificant, this investment helps minimize productivity losses and ensures proper system adoption. Prioritizing education funds leads to long-term optimization.
Challenges in EHR Onboarding and Training
Despite the numerous benefits of EHR systems, healthcare organizations often face significant challenges during the onboarding and training process. These challenges can impede the successful implementation and utilization of electronic health records. Some of the key challenges include:
- Change Resistance: Transitioning from paper-based systems can be met with reluctance as staff may feel comfortable with the familiar method, leading to slow adoption.
- Complexity: EHR systems often boast a multitude of features, requiring significant time and effort for staff to become proficient, potentially delaying the integration process.
- Time Constraints: Balancing patient care responsibilities with training sessions can be challenging, especially for busy healthcare professionals who have limited time available for additional learning activities.
- Costs: Implementing comprehensive training programs incurs expenses related to hiring trainers, developing customized content, and allocating staff resources for training sessions, which can strain budgets.
- Staff Turnover: High turnover rates necessitate frequent onboarding efforts, posing a challenge in maintaining consistent levels of EHR proficiency among staff members and potentially disrupting workflow efficiency.
Overcoming the Challenges
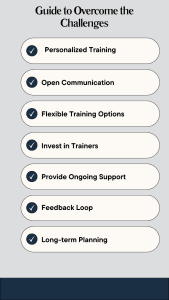
Here’s how to tackle these obstacles head-on:
- Personalized Training: Customize programs to fit different roles and learning styles.
- Open Communication: Address concerns openly and highlight the benefits of EHR adoption.
- Flexible Training Options: Offer various training formats to accommodate different schedules and preferences.
- Invest in Trainers: Support trainer development to ensure effective delivery of training.
- Provide Ongoing Support: Offer continued support and resources beyond initial training sessions.
- Feedback Loop: Regularly gather feedback to improve training methods and address gaps.
- Long-term Planning: Develop a sustainable plan for ongoing training and support.
By recognizing these challenges and implementing tailored solutions, healthcare organizations can ensure a smoother transition to EHR systems and reap the benefits they offer for patient care.
In Summary
Comprehensive training and onboarding ensure staff have the skills, support, and adaptability to leverage your EHR system meaningfully. Investing in role-based education, phased learning, robust evaluation, and ongoing development is crucial to realizing the transformational potential of electronic health records for your patients and organization.
Addressing Key Questions on EHR Training
With the framework to deliver robust EHR training covered, you may still have some common queries. Here are answers to some frequently asked questions:
1. How long does it take for staff to become proficient in a new EHR system?
It varies based on complexity and prior experience, but on average, 8-12 weeks of training are needed from software installation to go-live proficiency.
2. How do you identify and train EHR super-users?
Look for tech-savvy staff enthusiastic about the system. Have them train first through vendor-led boot camps before conducting peer training. Compensate them for extra responsibilities.
3. What are some key metrics to track training effectiveness?
- Course completion rates: Percentage of assigned modules finished
- Test scores: Demonstrated knowledge and skill acquisition
- Workflow adherence: Audit staff on process compliance
- Patient chart accuracy: Review charts for completeness
- End-user satisfaction surveys: Feedback on training experience
4. How can you minimize productivity loss during training?
To minimize productivity loss during training, several strategies can be implemented. Firstly, cross-training staff to cover multiple functions ensures that essential tasks are still carried out efficiently during training periods. Additionally, limiting training group sizes allows for more personalized attention and better engagement.
Conducting training in stages, rather than all at once, enables staff to gradually acclimate to the new system without overwhelming them. Providing post-go-live support through the transition phase ensures that staff have assistance readily available as they adjust to using the EHR system in real-world scenarios.
5. What are strategies to sustain proficiency post-implementation?
Sustaining proficiency post-implementation requires ongoing support and reinforcement. This includes refresher courses to revisit key concepts, job aids like cheat sheets for quick reference, and continuous performance assessments to identify knowledge gaps. Additionally, maintaining an EHR newsletter or blog highlighting new features and best practices ensures staff remain informed and engaged with the system.